Dementie patienten worden in de steek gelaten door oude tech oplossingen
Dr. Harro Stokman, CEO van Kepler Vision Technologies legt uit waarom bestaande technologische oplossingen mensen met dementie, deze patienten teleurstellen.

Caring for people with dementia is an extremely complicated issue. Whether living at home or in a care home, the condition presents a myriad of challenges to those suffering from it and to those responsible for caring for them.
Dementia can be confusing and debilitating, but good dementia care can support older people in living dignified and interesting lives at every stage of their condition.
Increasingly we’re seeing technology play a central role in helping those struggling with dementia to experience a higher quality of life for longer.
The scale of the problem certainly demands solutions that can work on the broadest possible scale.
In the UK, almost one million people are thought to have dementia, with the estimated cost to the UK economy of supporting people with this condition more than £34.7 billion.
These figures are predicted to rise in line with the aging population. Combined with the ongoing staffing crisis in the care sector, the need for better solutions is all the more urgent. 63% of those supporting a person with dementia say they don’t have enough support, representing a huge toll on frontline carers.
As with many areas of healthcare, new tech innovations have emerged which can ease the difficulties experienced by caregivers and help keep those diagnosed more comfortable and safe.
It would be impossible to summarise all of them here, but one area where dementia patients are being let down is in how they are monitored. How patients’ symptoms, their wellbeing, and even their location are monitored should form the foundation of what attention and treatment they receive, and what quality of life they can enjoy.
Many existing systems struggle with balancing the best possible care with allowing sufferers a degree of independence and dignity.
Take for example systems used to limit patient wandering in care-home or assisted living facilities. The old way of limiting the risk of this would be a combination of staff in-person monitoring and confining patients to specific rooms or areas – neither of which are ideal.
In-person monitoring by staff is incredibly inefficient and detracts from their core role of providing in-person care. Confining patients to certain locations deprives them of any ability to act independently, and, as a result, can prompt them to express frustration and despair.
According to the Alzheimer’s Association, 6 out of 10 people with dementia will wander off in response to fear, stress, looking to meet their basic needs, or even trying to retread old routines – which underlines the reasoning behind confinement.
But the trade-off is too one-sided. Wearables and similar tech appear to provide a potential solution to this.
Wristbands that are able to keep track of an individual’s geolocation, activity levels, and other metrics can offer carers advantages beyond just knowing where a patient is when they can’t be immediately found.
But wearable devices like electronic tags that are in contact with the body are often accused of causing further distress and discomfort, as well as lacking self-respect. Not to mention their usefulness is completely negated if a patient decides to simply take them off.
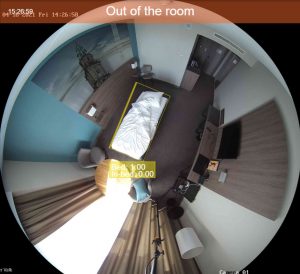
Another common tool used to monitor patients suffering from dementia is of course camera systems.
Present in many care homes and in an increasing number of personal homes where dementia sufferers continue to live independently, some carers find it brings peace of mind if they can see their loved one on a camera.
It can also help review the reasons for incidents, like falls or provide examples of physical discomfort.
But this raises the issue of privacy, and exactly how much of an invasion of privacy is acceptable to ensure someone’s wellbeing. Combining CCTV monitoring with GPS tracking may cover all of the bases when it comes to being able to find and easily help a person with dementia (whether at home or in a facility) but it can seem to many quite dehumanizing.
Technology for dementia patients must be designed specifically with the patients in mind. It needs to maximize the potential good while limiting the potential confusion and distress it might cause, without putting any additional burden on care staff.
This is where the combination of cutting-edge AI and basic low-tech modifications can do the most good. For example, better use of camera monitoring can be achieved with computer vision.
This AI-powered solution can monitor a patient’s location in a care facility without needing to tie up a member of staff by looking at dozens or even hundreds of video feeds.
No one can watch another person every second of the day, but an AI-powered video monitoring system can. Essentially, video feeds can be watched by programs in the cloud and can alert staff when there is a problem – for example when a patient is trying to access an area they are not supposed to, or to leave a location.
This kind of system can be integrated with IoT devices, like electronic door locks and devices used for staff alerts, to create a more subtle but still secure system of making sure patients with dementia do not wander off. As an added advantage, computer vision systems like this can often be deployed with other functionalities, like fall detection and the ability to signal staff when a patient is experiencing physical distress – helping to take care of their physical well-being as well as simply preventing worst-case scenarios.
A successful monitoring solution for dementia patients needs to be inexpensive, simple, user-friendly, easily standardized, and widely available to caregivers so that they are not only able to monitor patients in real-time, but so that they can help them recognize behavioral patterns that could inform their treatment. By using tools that maximize the safety of patients while limiting the potential for agitation or distress, caregivers can be given back the time needed to focus on their core role – providing the in-person engagement that patients with dementia need to live healthily and happy lives.
This article was also published here on Social Care Today